
International Society of Urological Pathology
Author: Kenneth A Iczkowski, MD University of California-Davis Health, USA
72-year-old man with distal penile lesion
You voted:
Both (squamous cell in the first and urothelial in the second)
Diagnosis by author:
Urothelial carcinoma in situ
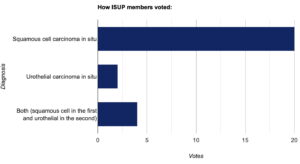
The dermatopathologist’s diagnosis was squamous cell carcinoma in situ.
A second specimen was received 5 weeks later consisting of a “distal urethral” biopsy (few 1- mm fragments of tissue) and a transurethral resection of a papillary lesion with multiple fragments up to 3 mm. The second specimen was much more consistent with non-invasive papillary urotheial carcinoma, high grade (grade 2 of 3) (Fig. 1). Rarely, however, the specimen showed a keratin pearl (Fig. 2). Immunostaining showed this tumor to be positive for cytokeratin 7, GATA-3 and p16 (Fig. 3) throughout.
Slides of the prior specimen was retrieved from the Dermatopathology department. After comparison with the current one, and after immunostaining of both cases, the diagnosis of the previous specimen was altered to “Urothelial carcinoma in situ with lateral spread.”
CLICK IMAGE TO ENLARGE
Discussion of case
It is obvious that the first specimen showed a transition from normal squamous epithelium to urothelial carcinoma. GATA-3 should usually be negative in squamous epithelium [3] but it was not here. The tendency toward nonspecificity of GATA-3 may explain why it stained both the neoplastic urothelial cells and non-neoplastic squamous epithelium.
In the urethra, carcinoma is more common in women than men. The main histologic type is urothelial carcinoma (54-65%), with squamous cell carcinoma a distant second (16-22%) and then adenocarcinoma (10-16%) [1]. However, in the bulbous and membranous portions of the (distal) male urethra, squamous cell carcinoma becomes more common and these are rarely associated with bladder tumors. These distal tumors have a better prognosis than proximal ones [2].
For this patient, glansectomy versus laser and topical treatment were considered based on the squamous cell diagnosis. For urothelial carcinoma in the same location, topical treatment and laser would likely not be effective because they would not reach inside the urethral bulb, from where the tumor eminated.
Key differential diagnosis
Squamous cell carcinoma: The first case had some resemblance to squamous cell carcinoma, so without immunostains it is easy to see how that diagnosis was made. However, the lesion showed a sharp transition to areas that were GATA-3 positive, p16 positive, and cytokeratin 7 positive. Skin is normally not cytokeratin 7 positive.
Urothelial carcinoma with lateral spread: The presence of papillary urothelial carcinoma in an adjacent topographic location made it unlikely that the patient would have two primary cancers.
Other urethral lesions include adenocarcinoma, in both sexes anywhere along the urethra, and clear cell adenocarcinoma, mostly in women and showing an association with urethral diverticulum.
Summary of clinical history
This 72-year-old man had a lesion at the penile urethral meatus that had been present for more than 2 years with some pain. Cystoscopy showed normal bladder and prostate. A biopsy was sent to the dermatopathologist. After their diagnosis, glansectomy versus laser and topical treatment were considered.
Gross findings
Designated, skin, urethral meatus were 4 tissue fragments ranging from 2 to 3 mm (Fig. 1).
Microscopic findings
The tissues showed a sharp transition between normal-thickness squamous appearing epithelium and thickened irregular areas with atypical cells, parakeratosis and hemorrhage (Fig. 2)
Immunohistochemical findings
Immunohistochemistry on the current specimen was not done until after a second specimen was received 5 weeks later.
P16 was reactive in the thickened area only (Fig. 3)
Cytokeratin 7 also was reactive in the thickened area (Fig. 4)
GATA-3 showed sparse nuclear reactivity throughout.
CLICK IMAGE TO ENLARGE