
International Society of Urological Pathology
Author: Dr Chara Ntala, St George’s University Hospital; Dr Wael Al-Qsous, NHS Lothian; Dr Marie O’Donnell, NHS Lothian
50-year-old female with visible hematuria
Discussion of case
Malakoplakia (from the Greek word malakos=soft and plaka= plaque) is a relatively rare acquired granulomatous disorder that was first described in the bladder by Michaelis and Gutmann in 1902. It occurs more commonly in the genitourinary tract (mostly in the bladder) and there is a female predominance. It has also been described in other locations including the gastrointestinal tract, skin, pancreas oropharynx, lymph nodes and retroperitoneum.
Histological examination shows sheets of eosinophilic histiocytes (Hansemann cells), intermingled with lymphocytes, plasma cells and neutrophils. There is an accumulation of Michaelis-Gutmann bodies, which are pathognomonic but not necessary for diagnosis. These are intracellular and extracellular concentrically laminated, round to ovoid, basophilic inclusions which are highlighted with von Kossa, periodic-acid–Schiff, Prussian blue, and Perl’s iron special stains. These are helpful in differentiating this condition from xanthogranulomatous and granulomatous cystitis.
The exact etiology of bladder malakoplakia remains unclear although its pathogenesis has three main hypotheses. Firstly, it is postulated that microorganisms might play a role in the, especially Escherichia Coli infection, which can have a long history of chronic urinary tract infections. Secondly, an abnormal or altered immune response has also been implicated as it has a higher incidence in patients having immunosuppressive diseases or long-term chronic diseases, such as HIV infection, tuberculosis, sarcoma, diabetes, and ulcerative colitis. Hematological malignancies, including chronic lymphocytic leukemia (CLL) are frequently associated with impairment of the immune system and are characterized, in some cases, by immune dysregulation. Notably, malakoplakia has been reported in CLL patients using drugs with a severe immunosuppressive effect before. The third hypothesis is an abnormal macrophage response because of defective phagolysosomal activity. It is suggested that macrophages in malakoplakia are capable of phagocytosis but unable to digest the bacteria, therefore partially digested bacteria accumulate in monocytes or macrophages and lead to the deposition of calcium and iron in the formation of basophilic structures, the Michaelis- Gutmann bodies.
The most common complication is hydroureteronephrosis, particularly when the lesion is located at was the vesicoureteral junction. Antibiotic therapy alone or in combination with surgery (TURBT or rarely partial cystectomy) provide the best therapeutic approach to avoid recurrences bladder malakoplakia (References 1–3).
References
Summary of clinical history
50-year-old female with visible hematuria underwent cystoscopy for possible early papillary areas, bladder biopsies were taken
Microscopic findings
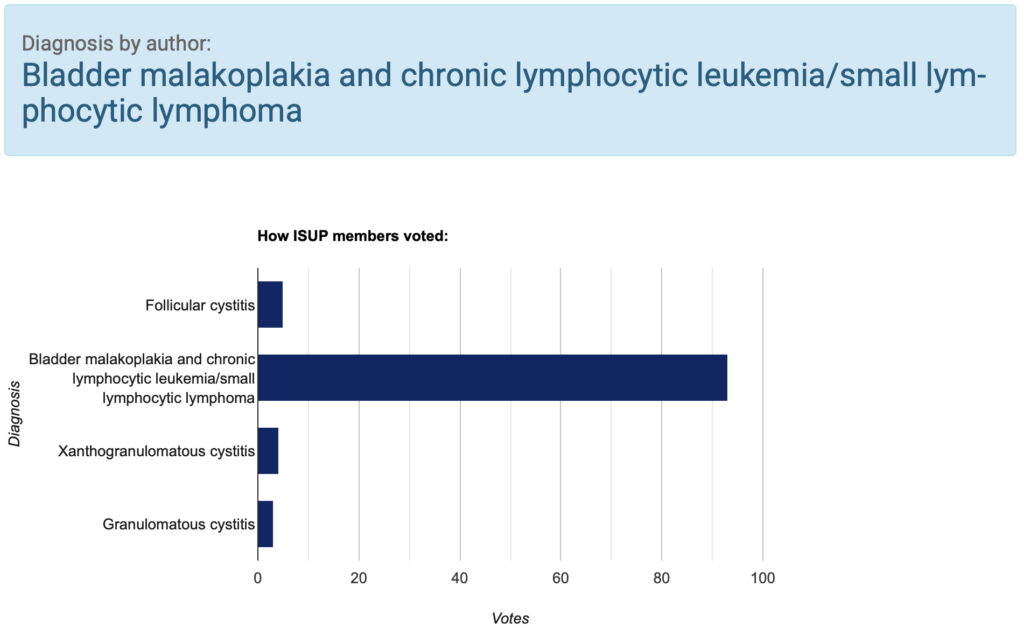
Histological examination showed lamina propria with a monotonous small lymphoid cell population in a diffuse and perivascular distribution. The lymphoid cells had minimal cytoplasm and central small round nuclei. Adjacent to this, there were aggregates of eosinophilic epithelioid histiocytes with Michaelis-Gutmann bodies (Figures 1-4). These were highlighted with von Kossa stain (Figure 5). Overlying urothelium was unremarkable with no evidence of CIS or malignancy.
CLICK IMAGE TO ENLARGE